‘Not for the faint of heart’
Capstan Medical’s structural heart robotic surgery system [Image courtesy of Capstan Medical]
Capstan Medical CEO Maggie Nixon says the surgical robotics developer is “driving hard” toward its first-in-human mitral heart valve replacement — and already has its sights set on tricuspid and aortic procedures.
“We have a novel implant, a catheter and a robotic platform,” she said in an interview with Medical Design & Outsourcing. “This is not for the faint of heart.”
Nixon joined Santa Cruz, California-based Capstan in 2022 after more than two decades as an engineer and executive at Intuitive to reunite with her first boss from Intuitive, Capstan founder and Chief Technology Officer Dan Wallace.
The two became friends over the decades as Wallace founded Hansen Medical with Intuitive co-founder Dr. Fred Moll and sold it for $80 million to Auris, which then sold to Johnson & Johnson MedTech for more than $3 billion in 2019.
“In 2022, he called me up and said, ‘Maggie, this is it. This is what we’re going to work on together. … I’m not even going to talk about it. Just come in and meet the team,’” Nixon said.
In Santa Cruz, she learned they developed a compact, catheter-delivered mitral valve implant but needed a robotics system to place it. She became CEO of Capstan’s incubator, Occam Labs, in 2022 and transitioned to Capstan’s full-time CEO in 2023.
“Our first hire in the robotic space was in June 2022 and we had an operational robot by December,” Nixon said. “We also very quickly realized while this was fundamentally enabling for mitral valve, this is a platform that can broadly serve structural heart. And that’s how we’ve evolved over the last couple of years. If you’ve got a capable system that can drive a portfolio of catheters and deploy a portfolio of implants, you’ve got a different, comprehensive solution for structural heart.”
Bigger than Intuitive?

Capstan Capstan founder and Chief Technology Officer Dan Wallace and CEO Maggie Nixon [Photo courtesy of Capstan Medical]
Initially intended as a surgical robotics system for cardiac procedures, Intuitive’s first da Vinci system found popularity among urologists for minimally invasive prostatectomies, setting the company on a different path toward soft-tissue surgical robotics dominance.
Nixon was on Intuitive’s original cardiac team as an instrument design engineer working on devices for revascularization and mitral valve repair. Her products have mostly since been retired from the portfolio as Intuitive pivoted. But all these years later, she remained passionate about minimally invasive heart surgery.
“Mitral valve is still only being treated 2.4% of the time, and that means there’s an immense number of patients out there that are looking for options, and looking for options that aren’t open-heart surgery,” Nixon said. “We were trying to do minimally invasive mitral valve repair back in 2000, and now here we are in 2024 about to do minimally invasive, no stopped-heart femoral access transseptal [replacement].”
Capstan Medical has its system locked down in a design freeze for verification and validation in the “flat-out sprint” to first-in-human on its mitral valve procedure, Nixon said, with hopes of starting a pivotal trial in 2026 and submission to the FDA for regulatory approval as soon as 2028.
“We’ve got this mitral valve — we’re locked and loaded and we’re moving forward — but there’s this opportunity sitting behind it,” Nixon said. “We’ve got a tricuspid valve that’s ready to go into full development mode. It’s already gone through first proof of concept. So we’ll be taking that off the shelf and driving that forward as well.”
Capstan sees a market that’s bigger than Intuitive Surgical’s, citing the fact that structural heart is the largest and fastest growing segment of the medical device industry.
“Compared to when I started at Intuitive back in 2000 where I was laughed out of the room by clinicians for a decade, it’s been really fun to engage with these cardiologists,” Nixon said. “I expected a massive, ‘Yeah, we don’t need robotics’ sort of mentality. It couldn’t be more opposite. The vast majority of cardiologists that I’ve been talking to are saying, ‘It’s about time.’”
The company hopes for FDA breakthrough device designation on its mitral product to fast-track pre-market approval — and accelerated procedure reimbursement to bankroll expansion into other cardiac procedures.
Capstan’s mitral valve technology

Capstan Medical’s mitral valve implant [Photo courtesy of Capstan Medical]
Nixon recalled the first time she got her hand on the mitral valve implant and delivery catheter, which she operated manually on the bench top.
“There is an amazing mechanism for slow and controlled deployment, and the catheter has multiple degrees of freedom to very accurately and precisely position it into the annulus,” she said.
The valve implant is designed with a rigid 35 mm length and an outer diameter of less than 31 French when compressed inside the catheter. That short length increases control during placement, while the diameter is meant to minimize vascular and septal trauma.
The valve uses nitinol tines to anchor the device. Two rows of tines provide redundancy. For long-term retention, a woven fabric covering encourages tissue integration.
The mitral valve has a ventricular depth of less than 10 mm to minimize the potential for obstruction, which is the main reason that a patient wouldn’t be eligible for a minimally invasive mitral valve replacement.
“One thing that we’re really focusing on is inclusion. A lot of the devices that are in clinical studies have a massive exclusion, in [the range of] 70% to 90% on some of these devices,” Nixon said. “One of the things that we’ve been trying to do with the platform and our implant is if you’ve got a really precise and controlled delivery system, you can make a really compact implant that resolves some of what’s driving this exclusion.”
The predominant driver of exclusions is left ventricular outflow tract (LVOT) obstruction, where larger valves can block that outflow tract when anchoring in the annulus. And large anchoring systems are sometimes needed to secure valves lacking precise placement.
For Capstan, the solution for inclusion came with the combination of a compact implant and precise placement.
“This is where those two things came together,” Nixon said. “We put the implant team and the delivery system teams shoulder to shoulder, and they were working through how to to optimize both. We’ve been looking hard at the images of patients that have been excluded from trials … and what do we need to do on the implant to serve those patients, and then what do we need to do on the delivery system to make it possible.”
The second leading driver of exclusions is when a patient’s vascular system isn’t large enough to allow the device through a catheter — which is why Capstan is working to slim its device down even further to 28 French — followed by mitral annulus calcification (MAC).
“You’ll see a lot of these trials have had these arms being added to address calcified annulus. If you’re oversizing your valve significantly in order to retain it, it may not be compatible if you’ve got calcifications in there,” Nixon said. “We’ve got a soft outer body of our valve, and a very rigid inner core. The rigid inner core protects the leaflets, makes them highly reliable, but then we’ve optimized our nitinol retention mechanisms to be very soft and compliant so they can conform to the calcified annulus in a different way.”
Overcoming these exclusion issues could help Capstan Medical move through its pivotal trial faster than would otherwise be expected, she said. The company is starting with a single size of mitral valve, with two more sizes likely to follow.
“We think we hit the middle of the curve,” Nixon said. “We’ve assessed so many CT images, and we think we’ll need one bigger and one smaller, but that’s something that will evolve as we go through our screening of our patients in our clinical activity. We’re working on the one up right now, and then we’ll decide whether it’s another one on the upside, or if we need one on the smaller side.”
Capstan’s delivery catheter technology

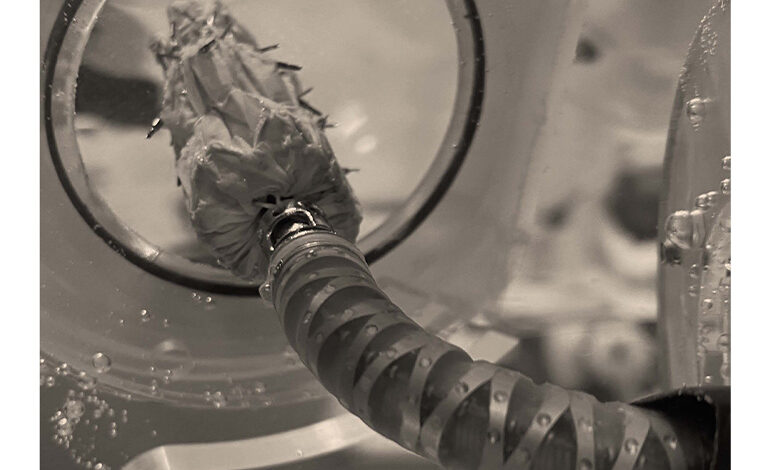
This photo shows the articulated end of Capstan Medical’s delivery catheter and the compressed mitral valve implant. [Photo courtesy of Capstan Medical]
Capstan Medical’s name comes from a key feature on the delivery catheter that works like the capstan winch on a sailboat, offering a unique way to control expansion of the implant inside the heart.
Other catheter-delivered devices use nitinol’s superelastic properties to self-expand as soon as they’re freed from the compressing force of a delivery catheter’s sheath.
“We have a novel mechanism at the end of our catheter that cinches the implant down from the inside, completely decoupling the sheath from the implant deployment,” Nixon said. “So you pull the sheath back, your implant is still collapsed. When you want to open it up a little bit and fine tune your positioning, you still have full control and can open it up a little bit more.”
Nixon said the disposable delivery catheters don’t use the more familiar tube-in-tube technology, but instead have “discrete articulating linkages at the end … similar to what you see in in more robotic-type instruments.”
These cable-driven, metal linkages optimize range of motion for precise control and placement of the implant. Cardiologists performing the first-in-human cases will use fluroscopy and echocardiogaphy imaging while operating the robot with a Microsoft Xbox controller. For femoral access, the equipment advancing the catheter will sit next to the patient’s leg.
“It’s attached to the table, clutches out of the way when you don’t need it, then pops up by the patient’s thigh,” Nixon said. “They put the sheath in to access and then you you insert your catheter, dock it to the robot and then drive it into position.”
The biggest challenge
“The complexity at Capstan Medical comes from the fact that we’re not just an implant company, not just a catheter company, not just a robot company. We’re kind of all three mixed in together, which makes us look a little bit different but also is where the capability comes from,” Nixon said. “None of those have been developed in isolation — they’re developed concurrently. A lot of people take a little bit of time to think through how that technology stack can be enabling, and not just the tech in each one of those areas.”
Nixon said she and Wallace are staying vigilant about feature creep given all the potential for their technology. For example, they know they can design the system to collapse the implant back down after it’s been deployed, but are working with doctors to determine whether that feature is critical enough to justify the additional complexity.
“There’s so many things we could do, but if it’s not anchored in what we’re seeking to solve for, it’s not worth it right now,” Nixon said. “The team has done such an amazing job of deeply understanding the clinical problem that we’re solving for, and we’ve got all of these amazing things that would be super cool. But if they’re not core to solving that problem right now, they’re distractions.”
“Dan and I spend a good chunk of our mental load making sure that we’re picking the right things to keep in,” she continued. “That doesn’t mean that we’re not thinking about what would be awesome [in the] future. We just want to stay true to what must be done in order to solve the clinical problem.”