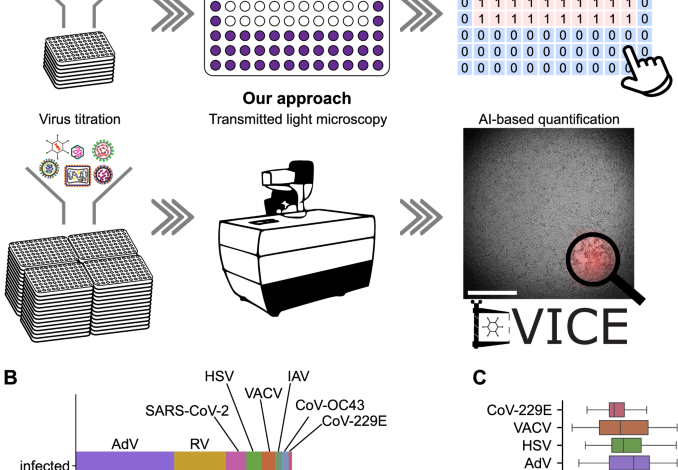
A versatile automated pipeline for quantifying virus infectivity by label-free light microscopy and artificial intelligence
Moriyama, M., Hugentobler, W. J. & Iwasaki, A. Seasonality of respiratory viral infections. Annu. Rev. Virol. 7, 83–101 (2020).
Virgin, H. W. The virome in mammalian physiology and disease. Cell 157, 142–150 (2014).
Prasad, V. & Greber, U. F. The endoplasmic reticulum unfolded protein response— homeostasis, cell death and evolution in virus infections. FEMS Microbiol. Rev. 45, fuab016 (2021).
Netherton, C., Moffat, K., Brooks, E. & Wileman, T. A guide to viral inclusions, membrane rearrangements, factories, and viroplasm produced during virus replication. Adv. Virus Res. 70, 101–182 (2007).
Leland, D. S. & Ginocchio, C. C. Role of cell culture for virus detection in the age of technology. Clin. Microbiol. Rev. 20, 49–78 (2007).
Dulbecco, R. Production of plaques in monolayer tissue cultures by single particles of an animal virus. Proc. Natl Acad. Sci. USA 38, 747–752 (1952).
Reed, L. J. & Muench, H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 27, 493–497 (1938).
Smither, S. J. et al. Comparison of the plaque assay and 50% tissue culture infectious dose assay as methods for measuring filovirus infectivity. J. Virol. Methods 193, 565–571 (2013).
Keiser, P. T., Anantpadma, M., Staples, H., Carrion, R. & Davey, R. A. Automation of infectious focus assay for determination of filovirus titers and direct comparison to plaque and TCID50 assays. Microorganisms 9, 156 (2021).
Saotome, K., Morita, H. & Umeda, M. Cytotoxicity test with simplified crystal violet staining method using microtitre plates and its application to injection drugs. Toxicol. Vitr. 3, 317–321 (1989).
Yakimovich, A. et al. Inhibition of poxvirus gene expression and genome replication by bisbenzimide derivatives. J. Virol. 91, e00838-17 (2017).
Yakimovich, A. et al. Cell-free transmission of human adenovirus by passive mass transfer in cell culture simulated in a computer model. J. Virol. 86, 10123–10137 (2012).
Prasad, A. & Alizadeh, E. Cell form and function: interpreting and controlling the shape of adherent cells. Trends Biotechnol. 37, 347–357 (2019).
Witte, R., Andriasyan, V., Georgi, F., Yakimovich, A. & Greber, U. F. Concepts in light microscopy of viruses. Viruses 10, 202 (2018).
Suomalainen, M. & Greber, U. F. Virus infection variability by single-cell profiling. Viruses 13, 1568 (2021).
Petkidis, A., Andriasyan, V. & Greber, U. F. Label-free microscopy for virus infections. Reprod. Syst. Sex. Disord. 72, 204–212 (2023).
Moen, E. et al. Deep learning for cellular image analysis. Nat. Methods 16, 1233–1246 (2019).
Petkidis, A., Andriasyan, V. & Greber, U. F. Machine learning for cross-scale microscopy of viruses. Cell Rep. Methods 3, 100557 (2023).
Christiansen, E. M. et al. In silico labeling: predicting fluorescent labels in unlabeled images. Cell 173, 792–803.e19 (2018).
Ounkomol, C., Seshamani, S., Maleckar, M. M., Collman, F. & Johnson, G. R. Label-free prediction of three-dimensional fluorescence images from transmitted-light microscopy. Nat. Methods 15, 917–920 (2018).
Kim, D., Min, Y., Oh, J. M. & Cho, Y.-K. AI-powered transmitted light microscopy for functional analysis of live cells. Sci. Rep. 9, 18428 (2019).
Hochdorfer, D., Businger, R., Hotter, D., Seifried, C. & Solzin, J. Automated, label-free TCID50 assay to determine the infectious titer of virus-based therapeutics. J. Virol. Methods 299, 114318 (2022).
Wang, T.-E. et al. Differentiation of cytopathic effects (CPE) induced by influenza virus infection using deep convolutional neural networks (CNN). PLoS Comput. Biol. 16, e1007883 (2020).
Chen, J.-J. et al. Detection of cytopathic effects induced by influenza, parainfluenza, and enterovirus using deep convolution neural network. Biomedicines 10, 70 (2022).
Dodkins, R. et al. A rapid, high throughput, viral infectivity assay using automated brightfield microscopy with machine learning. SLAS Technol. 28, 324–333 (2023).
Tan, M. & Le, Q. V. EfficientNet: rethinking model scaling for convolutional neural networks. Preprint at bioarXiv. https://arxiv.org/abs/1905.11946 (2019).
Murer, L. et al. Identification of broad anti-coronavirus chemical agents for repurposing against SARS-CoV-2 and variants of concern. Curr. Res. Virol. Sci. 3, 100019 (2022).
Barut, G. T. et al. The spike gene is a major determinant for the SARS-CoV-2 Omicron-BA.1 phenotype. Nat. Commun. 13, 5929 (2022).
Dalal, N. & Triggs, B. Histograms of oriented gradients for human detection. In 2005 IEEE Computer Society Conference on Computer Vision and Pattern Recognition (CVPR’05), vol. 1, 886–893 (IEEE, San Diego, CA, USA, 2005).
Cresta, D. et al. Time to revisit the endpoint dilution assay and to replace the TCID50 as a measure of a virus sample’s infection concentration. PLoS Comput. Biol. 17, e1009480 (2021).
Zhou, B., Khosla, A., Lapedriza, A., Oliva, A. & Torralba, A. Learning deep features for discriminative localization. In 2016 IEEE Conference on Computer Vision and Pattern Recognition (CVPR) 2921–2929 (IEEE, Las Vegas, NV, USA, 2016).
Jetzer, T., Studer, L., Bieri, M., Greber, U. & Hemmi, S. Engineered human adenoviruses of species B and C report early, intermediate early and late viral gene expression. Hum. Gene Ther. https://doi.org/10.1089/hum.2023.121 (2023).
Goodfellow, I., Bengio, Y. & Courville, A. Deep Learning (Adaptive Computation and Machine Learning series) 800 (The MIT Press, 2016).
Laine, R. F., Arganda-Carreras, I., Henriques, R. & Jacquemet, G. Avoiding a replication crisis in deep-learning-based bioimage analysis. Nat. Methods 18, 1136–1144 (2021).
Olszewski, D. et al. High-content, arrayed compound screens with rhinovirus, influenza A virus and herpes simplex virus infections. Sci. Data 9, 610 (2022).
Georgi, F. et al. The FDA-approved drug Nelfinavir inhibits lytic cell-free but not cell-associated nonlytic transmission of human adenovirus. Antimicrob. Agents Chemother. 64, e01002-20 (2020).
Shelley, M. & Krippendorff, K. Content analysis: an introduction to its methodology. J. Am. Stat. Assoc. 79, 240 (1984).
Wyllie, A. L. et al. Saliva or nasopharyngeal swab specimens for detection of SARS-CoV-2. N. Engl. J. Med. 383, 1283–1286 (2020).
Puhach, O. et al. Infectious viral load in unvaccinated and vaccinated individuals infected with ancestral, Delta or Omicron SARS-CoV-2. Nat. Med. 28, 1491–1500 (2022).
López-Ríos, F., Illei, P. B., Rusch, V. & Ladanyi, M. Evidence against a role for SV40 infection in human mesotheliomas and high risk of false-positive PCR results owing to presence of SV40 sequences in common laboratory plasmids. Lancet 364, 1157–1166 (2004).
Naccache, S. N. et al. The perils of pathogen discovery: origin of a novel parvovirus-like hybrid genome traced to nucleic acid extraction spin columns. J. Virol. 87, 11966–11977 (2013).
Nolte, F. S. et al. Evaluation of a rapid and completely automated real-time reverse transcriptase PCR assay for diagnosis of enteroviral meningitis. J. Clin. Microbiol. 49, 528–533 (2011).
Volle, R. et al. Methylene blue, Mycophenolic acid, Posaconazole, and Niclosamide inhibit SARS-CoV-2 Omicron variant BA.1 infection of human airway epithelial organoids. Curr. Res. Microb. Sci. 3, 100158 (2022).
Georgi, F. et al. A high-content image-based drug screen of clinical compounds against cell transmission of adenovirus. Sci. Data 7, 265 (2020).
Andriasyan, V. et al. Microscopy deep learning predicts virus infections and reveals mechanics of lytic-infected cells. iScience 24, 102543 (2021).
Yakimovich, A. et al. Plaque2.0—a high-throughput analysis framework to score virus-cell transmission and clonal cell expansion. PLoS ONE 10, e0138760 (2015).
Metsky, H. C. et al. Designing sensitive viral diagnostics with machine learning. Nat. Biotechnol. 40, 1123–1131 (2022).
Gutierrez, B., Escalera-Zamudio, M. & Pybus, O. G. Parallel molecular evolution and adaptation in viruses. Curr. Opin. Virol. 34, 90–96 (2019).
Ison, M. G. Antivirals and resistance: influenza virus. Curr. Opin. Virol. 1, 563–573 (2011).
Domingo, E., Escarmís, C., Lázaro, E. & Manrubia, S. C. Quasispecies dynamics and RNA virus extinction. Virus Res. 107, 129–139 (2005).
Murer, L., Petkidis, A., Vallet, T., Vignuzzi, M. & Greber, U. F. Chemical evolution of rhinovirus identifies capsid-destabilizing mutations driving low-ph-independent genome uncoating. J. Virol. 96, e0106021 (2022).
Khoury, D. S. et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat. Med. 27, 1205–1211 (2021).
Corti, D. & Lanzavecchia, A. Broadly neutralizing antiviral antibodies. Annu. Rev. Immunol. 31, 705–742 (2013).
Pan, S. J. & Yang, Q. A survey on transfer learning. IEEE Trans. Knowl. Data Eng. 22, 1345–1359 (2010).
Glauser, D. L. et al. Inhibition of herpes simplex virus type 1 replication by adeno-associated virus rep proteins depends on their combined DNA-binding and ATPase/helicase activities. J. Virol. 84, 3808–3824 (2010).
Crameri, M. et al. MxB is an interferon-induced restriction factor of human herpesviruses. Nat. Commun. 9, 1980 (2018).
Abadi, M. et al. TensorFlow: large-scale machine learning on heterogeneous distributed systems. Preprint at bioarXiv https://arxiv.org/abs/1603.04467 (2016).
Sandler, M., Howard, A., Zhu, M., Zhmoginov, A. & Chen, L.-C. Mobilenetv2: inverted residuals and linear bottlenecks. In 2018 IEEE/CVF Conference on Computer Vision and Pattern Recognition 4510–4520 (IEEE, 2018).
Hu, J., Shen, L., Albanie, S., Sun, G. & Wu, E. Squeeze-and-excitation networks. IEEE Trans. Pattern Anal. Mach. Intell. 42, 2011–2023 (2020).
van der Walt, S. et al. scikit-image: image processing in Python. PeerJ 2, e453 (2014).
Pedregosa, F., Varoquaux, G. & Gramfort, A. Scikit-learn: machine learning in Python. J. Mach. Learn. Res. 12, 2825–2830 (2011).
Berg, S. et al. ilastik: interactive machine learning for (bio)image analysis. Nat. Methods 16, 1226–1232 (2019).
Petkidis, A., Andriasyan, V., Murer, L., Volle, R. & Greber, U. DVICE: detection of virus-induced cytopathic effect using AI. Zenodo. https://doi.org/10.5281/zenodo.11397906 (2024).
Cervantes-Barragan, L. et al. Dendritic cell-specific antigen delivery by coronavirus vaccine vectors induces long-lasting protective antiviral and antitumor immunity. MBio. 1, e00171-10 (2010).



