Artificial intelligence in surgery | Nature Medicine
Mnih, V. et al. Human-level control through deep reinforcement learning. Nature 518, 529–533 (2015).
Wallace, M. B. et al. Impact of artificial intelligence on miss rate of colorectal neoplasia. Gastroenterology 163, 295–304.e5 (2022).
Sharma, P. & Hassan, C. Artificial intelligence and deep learning for upper gastrointestinal neoplasia. Gastroenterology 162, 1056–1066 (2022).
Aerts, H. J. W. L. The potential of radiomic-based phenotyping in precision medicine: a review. JAMA Oncol. 2, 1636–1642 (2016).
Esteva, A. et al. A guide to deep learning in healthcare. Nat. Med. 25, 24–29 (2019).
COVIDSurg Collaborative.Projecting COVID-19 disruption to elective surgery.Lancet 399, 233–234 (2022).
Weiser, T. G. et al. Estimate of the global volume of surgery in 2012: an assessment supporting improved health outcomes. Lancet 385, S11 (2015).
Meara, J. G. & Greenberg, S. L. M. The Lancet Commission on Global Surgery Global surgery 2030: evidence and solutions for achieving health, welfare and economic development. Surgery 157, 834–835 (2015).
Alkire, B. C. et al. Global access to surgical care: a modelling study. Lancet Glob. Health 3, e316–e323 (2015).
Grönroos-Korhonen, M. T. et al. Failure to rescue after reoperation for major complications of elective and emergency colorectal surgery: a population-based multicenter cohort study. Surgery 172, 1076–1084 (2022).
GlobalSurg Collaborative. Mortality of emergency abdominal surgery in high-, middle- and low-income countries.Br. J. Surg. 103, 971–988 (2016).
GlobalSurg Collaborative & National Institute for Health Research Global Health Research Unit on Global Surgery. Global variation in postoperative mortality and complications after cancer surgery: a multicentre, prospective cohort study in 82 countries. Lancet 397, 387–397 (2021).
GlobalSurg Collaborative. Surgical site infection after gastrointestinal surgery in high-income, middle-income, and low-income countries: a prospective, international, multicentre cohort study. Lancet Infect Dis. 18, 516–525 (2018).
Paton, F. et al. Effectiveness and implementation of enhanced recovery after surgery programmes: a rapid evidence synthesis. BMJ Open 4, e005015 (2014).
Vedula, S. S. & Hager, G. D. Surgical data science: the new knowledge domain. Innov. Surg. Sci. 2, 109–121 (2017).
Kaddour J. et al. Challenges and applications of large language models. Preprint at https://arxiv.org/abs/2307.10169 (2023).
Bonde, A. et al. Assessing the utility of deep neural networks in predicting postoperative surgical complications: a retrospective study. Lancet Digit. Health 3, e471–e485 (2021).
Gögenur, I. Introducing machine learning-based prediction models in the perioperative setting. Br. J. Surg. 110, 533–535 (2023).
Mascagni, P. et al. Computer vision in surgery: from potential to clinical value. NPJ Digit. Med. 5, 163 (2022).
Wijnberge, M. et al. Effect of a machine learning-derived early warning system for intraoperative hypotension vs standard care on depth and duration of intraoperative hypotension during elective noncardiac surgery: the HYPE randomized clinical trial. J. Am. Med. Assoc. 323, 1052–1060 (2020).
Kalidasan, V. et al. Wirelessly operated bioelectronic sutures for the monitoring of deep surgical wounds. Nat. Biomed. Eng. 5, 1217–1227 (2021).
Fazlollahi, A. M. et al. Effect of artificial intelligence tutoring vs expert instruction on learning simulated surgical skills among medical students: a randomized clinical trial. JAMA Netw. Open 5, e2149008 (2022).
Wells, C. I. et al. Wearable devices to monitor recovery after abdominal surgery: scoping review. BJS Open 6, zrac031 (2022).
Dawes, A. J., Lin, A. Y., Varghese, C., Russell, M. M. & Lin, A. Y. Mobile health technology for remote home monitoring after surgery: a meta-analysis. Br. J. Surg. 108, 1304–1314 (2021).
Loftus, T. J. et al. Artificial intelligence and surgical decision-making. JAMA Surg. 155, 148–158 (2020).
Safavi, K. C. et al. Development and validation of a machine learning model to aid discharge processes for inpatient surgical care. JAMA Netw. Open 2, e1917221 (2019).
Dundar, T. T. et al. Machine learning-based surgical planning for neurosurgery: artificial intelligent approaches to the cranium. Front. Surg. 9, 863633 (2022).
Sadeghi, A. H. et al. Virtual reality and artificial intelligence for 3-dimensional planning of lung segmentectomies. JTCVS Tech. 7, 309–321 (2021).
Zhang, T. et al. RadioLOGIC, a healthcare model for processing electronic health records and decision-making in breast disease. Cell Rep. Med. 4, 101131 (2023).
Korfiatis, P. et al. Automated artificial intelligence model trained on a large data set can detect pancreas cancer on diagnostic computed tomography scans as well as visually occult preinvasive cancer on prediagnostic computed tomography scans. Gastroenterology 165, 1533–1546.e4 (2023).
Maier-Hein, L. et al. Surgical data science for next-generation interventions. Nat. Biomed. Eng. 1, 691–696 (2017).
Verma, A., Agarwal, G., Gupta, A. K. & Sain, M. Novel hybrid intelligent secure cloud Internet of things based disease prediction and diagnosis. Electronics 10, 3013 (2021).
Ghaffar Nia, N., Kaplanoglu, E. & Nasab, A.Evaluation of artificial intelligence techniques in disease diagnosis and prediction.Discov. Artif. Intell. 3, 5 (2023).
Gong, D. et al. Detection of colorectal adenomas with a real-time computer-aided system (ENDOANGEL): a randomised controlled study. Lancet Gastroenterol. Hepatol. 5, 352–361 (2020).
Wang, P. et al. Effect of a deep-learning computer-aided detection system on adenoma detection during colonoscopy (CADe-DB trial): a double-blind randomised study. Lancet Gastroenterol. Hepatol. 5, 343–351 (2020).
Kiani, A. et al. Impact of a deep learning assistant on the histopathologic classification of liver cancer. NPJ Digit. Med. 3, 23 (2020).
Hosny, A., Parmar, C., Quackenbush, J., Schwartz, L. H. & Aerts, H. J. W. L. Artificial intelligence in radiology. Nat. Rev. Cancer 18, 500–510 (2018).
Dias, R. & Torkamani, A. Artificial intelligence in clinical and genomic diagnostics. Genome Med. 11, 70 (2019).
Rajpurkar, P., Chen, E., Banerjee, O. & Topol, E. J. AI in health and medicine. Nat. Med. 28, 31–38 (2022).
Javanmard-Emamghissi, H. & Moug, S. J. The virtual uncertainty of futility in emergency surgery. Br. J. Surg. 109, 1184–1185 (2022).
Ali, R. et al. Bridging the literacy gap for surgical consents: an AI–human expert collaborative approach. NPJ Digit. Med. 7, 63 (2024).
Vernooij, J. E. M. et al. Performance and usability of pre-operative prediction models for 30-day peri-operative mortality risk: a systematic review. Anaesthesia 78, 607–619 (2023).
Wynants, L. et al. Prediction models for diagnosis and prognosis of COVID-19: systematic review and critical appraisal. Br. Med. J. 369, m1328 (2020).
Finlayson, S. G., Beam, A. L. & van Smeden, M. Machine learning and statistics in clinical research articles—moving past the false dichotomy. JAMA Pediatr. 177, 448–450 (2023).
Chiew, C. J., Liu, N., Wong, T. H., Sim, Y. E. & Abdullah, H. R. Utilizing machine learning methods for preoperative prediction of postsurgical mortality and intensive care unit admission. Ann. Surg. 272, 1133–1139 (2020).
COVIDSurg Collaborative. Machine learning risk prediction of mortality for patients undergoing surgery with perioperative SARS-CoV-2: the COVIDSurg mortality score. Br. J. Surg. 108, 1274–1292 (2021).
Maurer, L. R. et al. Validation of the Al-based Predictive OpTimal Trees in Emergency Surgery Risk (POTTER) calculator in patients 65 years and older. Ann. Surg. 277, e8–e15 (2023).
El Hechi, M. W. et al. Validation of the artificial intelligence-based Predictive Optimal Trees in Emergency Surgery Risk (POTTER) calculator in emergency general surgery and emergency laparotomy patients. J. Am. Coll. Surg. 232, 912–919.e1 (2021).
Gebran, A. et al. POTTER-ICU: an artificial intelligence smartphone-accessible tool to predict the need for intensive care after emergency surgery. Surgery 172, 470–475 (2022).
Bihorac, A. et al. MySurgeryRisk: development and validation of a machine-learning risk algorithm for major complications and death after surgery. Ann. Surg. 269, 652–662 (2019).
Ren, Y. et al. Performance of a machine learning algorithm using electronic health record data to predict postoperative complications and report on a mobile platform. JAMA Netw. Open 5, e2211973 (2022).
Bertsimas, D., Dunn, J., Velmahos, G. C. & Kaafarani, H. M. A. Surgical risk is not linear: derivation and validation of a novel, user-friendly, and machine-learning-based Predictive OpTimal Trees in Emergency Surgery Risk (POTTER) calculator. Ann. Surg. 268, 574–583 (2018).
El Moheb, M. et al. Artificial intelligence versus surgeon gestalt in predicting risk of emergency general surgery. J. Trauma Acute Care Surg. 95, 565–572 (2023).
Jalali, A. et al. Deep learning for improved risk prediction in surgical outcomes. Sci. Rep. 10, 9289 (2020).
Han R. et al. Randomized controlled trials evaluating AI in clinical practice: a scoping evaluation. Preprint at bioRxiv https://doi.org/10.1101/2023.09.12.23295381 (2023).
Li, B. et al. Machine learning in vascular surgery: a systematic review and critical appraisal. NPJ Digit. Med. 5, 7 (2022).
Artificial intelligence assists surgeons’ decision making. ClinicalTrials.gov https://classic.clinicaltrials.gov/ct2/show/record/NCT04999007 (2024).
Liu, X., Cruz Rivera, S., Moher, D., Calvert, M. J. & Denniston, A. K., SPIRIT-AI & CONSORT-AI Working Group. Reporting guidelines for clinical trial reports for interventions involving artificial intelligence: the CONSORT-AI extension. Nat. Med. 26, 1364–1374 (2020).
Collins, G. S. et al. Protocol for development of a reporting guideline (TRIPOD-AI) and risk of bias tool (PROBAST-AI) for diagnostic and prognostic prediction model studies based on artificial intelligence. BMJ Open 11, e048008 (2021).
Heus, P. et al. Uniformity in measuring adherence to reporting guidelines: the example of TRIPOD for assessing completeness of reporting of prediction model studies. BMJ Open 9, e025611 (2019).
Vasey, B. et al. Reporting guideline for the early stage clinical evaluation of decision support systems driven by artificial intelligence: DECIDE-AI. Br. Med. J. 377, e070904 (2022).
Cacciamani, G. E. et al. PRISMA AI reporting guidelines for systematic reviews and meta-analyses on AI in healthcare. Nat. Med. 29, 14–15 (2023).
Wynter-Blyth, V. & Moorthy, K. Prehabilitation: preparing patients for surgery. Br. Med. J. 358, j3702 (2017).
Topol, E. J. As artificial intelligence goes multimodal, medical applications multiply. Science 381, adk6139 (2023).
Boehm, K. M., Khosravi, P., Vanguri, R., Gao, J. & Shah, S. P. Harnessing multimodal data integration to advance precision oncology. Nat. Rev. Cancer 22, 114–126 (2022).
Yao, X. et al. Artificial intelligence-enabled electrocardiograms for identification of patients with low ejection fraction: a pragmatic, randomized clinical trial. Nat. Med. 27, 815–819 (2021).
Attia, Z. I. et al. Screening for cardiac contractile dysfunction using an artificial intelligence-enabled electrocardiogram. Nat. Med. 25, 70–74 (2019).
Ouyang, D. et al. Electrocardiographic deep learning for predicting post-procedural mortality: a model development and validation study. Lancet Digit. Health 6, e70–e78 (2024).
Kung, T. H. et al. Performance of ChatGPT on USMLE: potential for AI-assisted medical education using large language models. PLoS Digit. Health 2, e0000198 (2023).
Matias Y. & Corrado, G. Our latest health AI research updates. Google Blog https://blog.google/technology/health/ai-llm-medpalm-research-thecheckup/ (2023).
Decker, H. et al. Large language model-based chatbot vs surgeon-generated informed consent documentation for common procedures. JAMA Netw. Open 6, e2336997 (2023).
Ayers, J. W. et al. Comparing physician and artificial intelligence chatbot responses to patient questions posted to a public social media forum. JAMA Intern. Med. 183, 589–596 (2023).
Ke, Y. et al. Development and testing of retrieval augmented generation in large language models—a case study report. Preprint at https://arxiv.org/abs/2402.01733 (2024).
Perry, A. AI will never convey the essence of human empathy. Nat. Hum. Behav. 7, 1808–1809 (2023).
Loveys, K., Sagar, M., Pickering, I. & Broadbent, E. A digital human for delivering a remote loneliness and stress intervention to at-risk younger and older adults during the COVID-19 pandemic: randomized pilot trial. JMIR Ment. Health 8, e31586 (2021).
Introducing GPTs. OpenAI https://openai.com/blog/introducing-gpts (2023).
How assistants work. OpenAI https://platform.openai.com/docs/assistants/how-it-works (2023).
Ouyang, H. Your next hospital bed might be at home. The New York Times https://www.nytimes.com/2023/01/26/magazine/hospital-at-home.html (2023).
Temple-Oberle, C., Yakaback, S., Webb, C., Assadzadeh, G. E. & Nelson, G. Effect of smartphone app postoperative home monitoring after oncologic surgery on quality of recovery: a randomized clinical trial. JAMA Surg. 158, 693–699 (2023).
März, K. et al. Toward knowledge-based liver surgery: holistic information processing for surgical decision support. Int. J. Comput. Assist. Radiol. Surg. 10, 749–759 (2015).
Thirunavukarasu, A. J. et al. Trialling a large language model (ChatGPT) in general practice with the applied knowledge test: observational study demonstrating opportunities and limitations in primary care. JMIR Med. Educ. 9, e46599 (2023).
Glaese, A. et al. Improving alignment of dialogue agents via targeted human judgements. Preprint at https://arxiv.org/abs/2209.14375 (2022).
Johri, S. et al. Testing the limits of language models: a conversational framework for medical AI assessment. Preprint at https://www.medrxiv.org/content/10.1101/2023.09.12.23295399v1 (2023).
Cacciamani, G. E., Collins, G. S. & Gill, I. S. ChatGPT: standard reporting guidelines for responsible use. Nature 618, 238 (2023).
Haver, H. L. et al. Appropriateness of breast cancer prevention and screening recommendations provided by ChatGPT. Radiology 307, e230424 (2023).
Birkmeyer, J. D. et al. Surgical skill and complication rates after bariatric surgery. N. Engl. J. Med. 369, 1434–1442 (2013).
Zhang, J. et al. Rapid and accurate intraoperative pathological diagnosis by artificial intelligence with deep learning technology. Med. Hypotheses 107, 98–99 (2017).
Vermeulen, C. et al. Ultra-fast deep-learned CNS tumour classification during surgery. Nature 622, 842–849 (2023).
Mascagni, P. et al. Early-stage clinical evaluation of real-time artificial intelligence assistance for laparoscopic cholecystectomy. Br. J. Surg. 111, znad353 (2023).
Moor, M. et al. Foundation models for generalist medical artificial intelligence. Nature 616, 259–265 (2023).
Bechara, A., Damasio, H., Tranel, D. & Damasio, A. R. Deciding advantageously before knowing the advantageous strategy. Science 275, 1293–1295 (1997).
Van der Ven, W. H. et al. One of the first validations of an artificial intelligence algorithm for clinical use: the impact on intraoperative hypotension prediction and clinical decision-making. Surgery 169, 1300–1303 (2021).
Hatib, F. et al. Machine-learning algorithm to predict hypotension based on high-fidelity arterial pressure waveform analysis. Anesthesiology 129, 663–674 (2018).
Schneck, E. et al. Hypotension prediction index based protocolized haemodynamic management reduces the incidence and duration of intraoperative hypotension in primary total hip arthroplasty: a single centre feasibility randomised blinded prospective interventional trial. J. Clin. Monit. Comput. 34, 1149–1158 (2020).
Aklilu, J. G. et al. Artificial intelligence identifies factors associated with blood loss and surgical experience in cholecystectomy. NEJM AI 1, AIoa2300088 (2024).
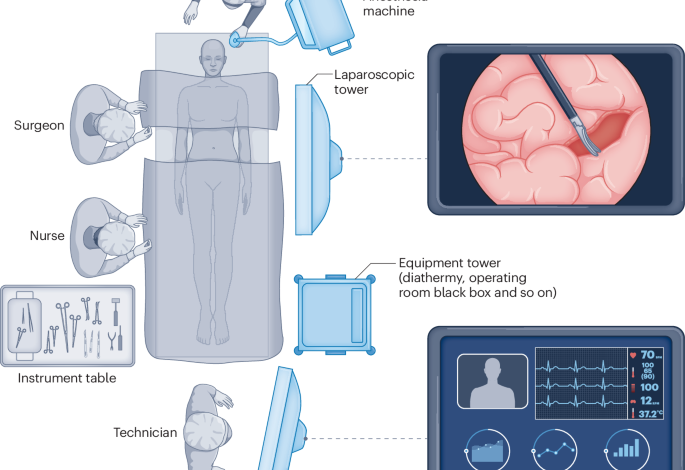
Jung, J. J., Jüni, P., Lebovic, G. & Grantcharov, T. First-year analysis of the operating room black box study. Ann. Surg. 271, 122–127 (2020).
Al Abbas, A. I. et al. The operating room black box: understanding adherence to surgical checklists. Ann. Surg. 276, 995–1001 (2022).
Seo, S. et al. Towards an AI coach to infer team mental model alignment in healthcare. IEEE Conf. Cogn. Comput. Asp. Situat. Manag. 2021, 39–44 (2021).
Agha, R. A., Fowler, A. J. & Sevdalis, N. The role of non-technical skills in surgery. Ann. Med Surg. 4, 422–427 (2015).
Gillespie, B. M. et al. Correlates of non-technical skills in surgery: a prospective study. BMJ Open 7, e014480 (2017).
Farrugia, G. Transforming health care through platforms. LinkedIn https://www.linkedin.com/pulse/transforming-health-care-through-platforms-gianrico-farrugia-m-d-/ (2023).
Feasibility and utility of artificial intelligence (AI)/machine learning (ML)—driven advanced intraoperative visualization and identification of critical anatomic structures and procedural phases in laparoscopic cholecystectomy. ClinicalTrials.gov https://classic.clinicaltrials.gov/ct2/show/NCT05775133?term=artificial+intelligence,+surgery&type=Intr&draw=2&rank=4 (2024).
Zia, A., Hung, A., Essa, I. & Jarc, A. Surgical activity recognition in robot-assisted radical prostatectomy using deep learning. In Medical Image Computing and Computer Assisted Intervention—MICCAI 2018 273–280 (Springer International Publishing, 2018).
Luongo, F., Hakim, R., Nguyen, J. H., Anandkumar, A. & Hung, A. J. Deep learning-based computer vision to recognize and classify suturing gestures in robot-assisted surgery. Surgery 169, 1240–1244 (2021).
Funke, I. et al. Using 3D convolutional neural networks to learn spatiotemporal features for automatic surgical gesture recognition in video. In Medical Image Computing and Computer Assisted Intervention—MICCAI 2019 467–475 (Springer International Publishing, 2019).
Lavanchy, J. L. et al. Automation of surgical skill assessment using a three-stage machine learning algorithm. Sci. Rep. 11, 5197 (2021).
Goodman E. D. et al. A real-time spatiotemporal AI model analyzes skill in open surgical videos. Preprint at https://arxiv.org/abs/2112.07219 (2021).
Kiyasseh, D. et al. A vision transformer for decoding surgeon activity from surgical videos. Nat. Biomed. Eng. 7, 780–796 (2023).
Goyal, P. et al. Vision models are more robust and fair when pretrained on uncurated images without supervision. Preprint at https://arxiv.org/abs/2202.08360 (2022).
Chatterjee, S., Bhattacharya, M., Pal, S., Lee, S.-S. & Chakraborty, C. ChatGPT and large language models in orthopedics: from education and surgery to research. J. Exp. Orthop. 10, 128 (2023).
Kim, J. S. et al. Can natural language processing and artificial intelligence automate the generation of billing codes from operative note dictations? Glob. Spine J. 13, 1946–1955 (2023).
Takeuchi, M. et al. Automated surgical-phase recognition for robot-assisted minimally invasive esophagectomy using artificial intelligence. Ann. Surg. Oncol. 29, 6847–6855 (2022).
Marcus, H. J. et al. The IDEAL framework for surgical robotics: development, comparative evaluation and long-term monitoring. Nat. Med. 30, 61–75 (2024).
Yip, M. et al. Artificial intelligence meets medical robotics. Science 381, 141–146 (2023).
Shademan, A. et al. Supervised autonomous robotic soft tissue surgery. Sci. Transl. Med. 8, 337ra64 (2016).
Hu, Y.-Y. et al. Complementing operating room teaching with video-based coaching. JAMA Surg. 152, 318–325 (2017).
Bonrath, E. M., Dedy, N. J., Gordon, L. E. & Grantcharov, T. P. Comprehensive surgical coaching enhances surgical skill in the operating room: a randomized controlled trial. Ann. Surg. 262, 205–212 (2015).
Goodman, E. D. et al. Analyzing surgical technique in diverse open surgical videos with multitask machine learning.JAMA Surg. 159, 185–192 (2024).
Levin, M., McKechnie, T., Khalid, S., Grantcharov, T. P. & Goldenberg, M. Automated methods of technical skill assessment in surgery: a systematic review. J. Surg. Educ. 76, 1629–1639 (2019).
Lam, K. et al. Machine learning for technical skill assessment in surgery: a systematic review. NPJ Digit. Med. 5, 24 (2022).
Kiyasseh, D. et al. A multi-institutional study using artificial intelligence to provide reliable and fair feedback to surgeons. Commun. Med. 3, 42 (2023).
Kiyasseh, D. et al. Human visual explanations mitigate bias in AI-based assessment of surgeon skills. NPJ Digit. Med. 6, 54 (2023).
Fazlollahi, A. M. et al. AI in surgical curriculum design and unintended outcomes for technical competencies in simulation training. JAMA Netw. Open 6, e2334658 (2023).
Artificial intelligence augmented training in skin cancer diagnostics for general practitioners (AISC-GP). ClinicalTrials.gov https://classic.clinicaltrials.gov/ct2/show/NCT04576416 (2024).
Testing the efficacy of an artificial intelligence real-time coaching system in comparison to in person expert instruction in surgical simulation training of medical students—a randomized controlled trial. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT05168150 (2024).
Knight, S. R. et al. Mobile devices and wearable technology for measuring patient outcomes after surgery: a systematic review. NPJ Digit. Med. 4, 157 (2021).
A clinical trial of the use of remote heart rhythm monitoring with a smartphone after cardiac surgery (SURGICAL-AF 2) ClinicalTrials.gov https://classic.clinicaltrials.gov/ct2/show/NCT05509517?term=artificial+intelligence,+surgery&recrs=e&type=Intr&draw=2&rank=14 (2024).
Sessler, D. I. & Saugel, B. Beyond ‘failure to rescue’: the time has come for continuous ward monitoring. Br. J. Anaesth. 122, 304–306 (2019).
Xu, W. et al. Continuous wireless postoperative monitoring using wearable devices: further device innovation is needed. Crit. Care 25, 394 (2021).
Bellini, V. et al. Machine learning in perioperative medicine: a systematic review. J. Anesth. Analg. Crit. Care 2, 2 (2022).
Junaid, M., Ali, S., Eid, F., El-Sappagh, S. & Abuhmed, T. Explainable machine learning models based on multimodal time-series data for the early detection of Parkinson’s disease. Comput. Methods Prog. Biomed. 234, 107495 (2023).
Lundberg, S. M. et al. Explainable machine-learning predictions for the prevention of hypoxaemia during surgery. Nat. Biomed. Eng. 2, 749–760 (2018).
Lu, S.-H. et al. Multimodal sensing and therapeutic systems for wound healing and management: a review. Sens. Actuators Rep. 4, 100075 (2022).
Anthis, A. H. C. et al. Modular stimuli-responsive hydrogel sealants for early gastrointestinal leak detection and containment. Nat. Commun. 13, 7311 (2022).
NIHR Global Health Research Unit on Global Surgery & GlobalSurg Collaborative Use of telemedicine for postdischarge assessment of the surgical wound: international cohort study, and systematic review with meta-analysis. Ann. Surg. 277, e1331–e1347 (2023).
McLean, K. A. et al. Evaluation of remote digital postoperative wound monitoring in routine surgical practice. NPJ Digit. Med. 6, 85 (2023).
Savage, N. Sibel Health: designing vital-sign sensors for delicate skin. Nature https://doi.org/10.1038/d41586-020-01806-7 (2020).
Callcut, R. A. et al. External validation of a novel signature of illness in continuous cardiorespiratory monitoring to detect early respiratory deterioration of ICU patients. Physiol. Meas. 42, 095006 (2021).
Shickel, B. et al. Dynamic predictions of postoperative complications from explainable, uncertainty-aware, and multi-task deep neural networks. Sci. Rep. 13, 1224 (2023).
Zhu, Y. et al. Prompting large language models for zero-shot clinical prediction with structured longitudinal electronic health record data. Preprint at https://arxiv.org/abs/2402.01713 (2024).
Xu, X. et al. A deep learning model for prediction of post hepatectomy liver failure after hemihepatectomy using preoperative contrast-enhanced computed tomography: a retrospective study. Front. Med. 10, 1154314 (2023).
Bhasker, N. et al. Prediction of clinically relevant postoperative pancreatic fistula using radiomic features and preoperative data. Sci. Rep. 13, 7506 (2023).
Ingwersen, E. W. et al. Radiomics preoperative-Fistula Risk Score (RAD-FRS) for pancreatoduodenectomy: development and external validation. BJS Open 7, zrad100 (2023).
Greijdanus, N. G. et al. Stoma-free survival after rectal cancer resection with anastomotic leakage: development and validation of a prediction model in a large international cohort. Ann. Surg. 278, 772–780 (2023).
Wells, C. I. et al. “Failure to rescue” following colorectal cancer resection: variation and improvements in a national study of postoperative mortality. Ann. Surg. 278, 87–95 (2022).
Smits, F. J. et al. Algorithm-based care versus usual care for the early recognition and management of complications after pancreatic resection in the Netherlands: an open-label, nationwide, stepped-wedge cluster-randomised trial.Lancet 399, 1867–1875 (2022).
Nepogodiev, D., Martin, J., Biccard, B., Makupe, A. & Bhangu, A. Global burden of postoperative death. Lancet 393, 401 (2019).
Dugan, R. E. & Gabriel, K. J. Changing the business of breakthroughs. Issues Sci. Technol. 38, 70–74 (2022).
Song, Y. et al. 3D-printed epifluidic electronic skin for machine learning-powered multimodal health surveillance. Sci. Adv. 9, eadi6492 (2023).
Kim, S., Brooks, A. K. & Groban, L. Preoperative assessment of the older surgical patient: honing in on geriatric syndromes. Clin. Inter. Aging 10, 13–27 (2015).
Kim, K. M., Yefimova, M., Lin, F. V., Jopling, J. K. & Hansen, E. N. A home-recovery surgical care model using AI-driven measures of activities of daily living. NEJM Catal. Innov. Care Deliv. (2022).
Modelling and AI using sensor data to personalise rehabilitation following joint replacement (MAPREHAB). ClinicalTrials.gov https://clinicaltrials.gov/study/NCT04289025 (2024).
Chen, E., Prakash, S., Janapa Reddi, V., Kim, D. & Rajpurkar, P. A framework for integrating artificial intelligence for clinical care with continuous therapeutic monitoring. Nat. Biomed. Eng. https://doi.org/10.1038/s41551-023-01115-0 (2023).
McLean, K. A. et al. Readiness for implementation of novel digital health interventions for postoperative monitoring: a systematic review and clinical innovation network analysis. Lancet Digit. Health 5, e295–e315 (2023).
Bilbro, N. A. et al. The IDEAL reporting guidelines: a Delphi consensus statement stage specific recommendations for reporting the evaluation of surgical innovation. Ann. Surg. 273, 82–85 (2021).
Skivington, K. et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. Br. Med. J. 374, n2061 (2021).
Horton, R. Surgical research or comic opera: questions, but few answers. Lancet 347, 984–985 (1996).
Bagenal, J. et al. Surgical research-comic opera no more. Lancet 402, 86–88 (2023).
Saeidi, H. et al. Autonomous robotic laparoscopic surgery for intestinal anastomosis. Sci. Robot 7, eabj2908 (2022).
Olavarria, O. A. et al. Robotic versus laparoscopic ventral hernia repair: multicenter, blinded randomized controlled trial. Br. Med. J. 370, m2457 (2020).
Kawka, M., Fong, Y. & Gall, T. M. H. Laparoscopic versus robotic abdominal and pelvic surgery: a systematic review of randomised controlled trials. Surg. Endosc. 37, 6672–6681 (2023).
Maier-Hein, L. et al. Surgical data science—from concepts toward clinical translation. Med. Image Anal. 76, 102306 (2022).
Janssen, B. V., Kazemier, G. & Besselink, M. G. The use of ChatGPT and other large language models in surgical science. BJS Open 7, zrad032 (2023).
Huang, Z., Bianchi, F., Yuksekgonul, M., Montine, T. J. & Zou, J. A visual-language foundation model for pathology image analysis using medical Twitter. Nat. Med. 29, 2307–2316 (2023).
Sandal, L. F. et al. Effectiveness of app-delivered, tailored self-management support for adults with lower back pain-related disability: a selfBACK randomized clinical trial. JAMA Intern. Med. 181, 1288–1296 (2021).
Strömblad, C. T. et al. Effect of a predictive model on planned surgical duration accuracy, patient wait time, and use of presurgical resources: a randomized clinical trial. JAMA Surg. 156, 315–321 (2021).
Auloge, P. et al. Augmented reality and artificial intelligence-based navigation during percutaneous vertebroplasty: a pilot randomised clinical trial. Eur. Spine J. 29, 1580–1589 (2020).
Tsoumpa, M. et al. The use of the Hypotension Prediction Index integrated in an algorithm of goal directed hemodynamic treatment during moderate and high-risk surgery. J. Clin. Med. 10, 5884 (2021).
Garrow, C. R. et al. Machine learning for surgical phase recognition. Ann. Surg. 273, 684–693 (2021).
Ramesh, A., Dhariwal, P., Nichol, A., Chu, C. & Chen, M. Hierarchical text-conditional image generation with CLIP latents. Preprint at https://arxiv.org/abs/2204.06125 (2022).
Vaswani, A. et al. Attention is all you need. In Advances in Neural Information Processing Systems 30 (NIPS, 2017).