FDA authorizes new drug to protect vulnerable from Covid-19

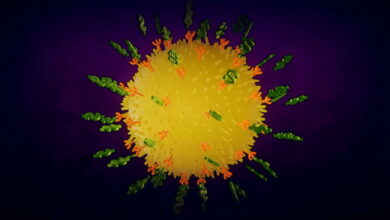
The Food and Drug Administration on Friday authorized a new antibody to protect immunocompromised individuals against Covid-19.
The drug, known as Pemgarda and marketed by the biotech Invivyd, is the first such drug to become available since the agency pulled AstraZeneca’s Evusheld off the market in January 2023. New Omicron variants had rendered Evusheld ineffective.
Some immunocompromised patients — a group that includes certain cancer patients, patients with some autoimmune or genetic disorders, and organ transplant recipients — have been eagerly awaiting the new prophylactic. Because their condition or drugs they take for it weaken their immune systems, they don’t always get adequate protection from vaccination. Antibody treatments can add additional protection.
There remains a need for additional Covid protections. Last week, over 10,000 patients with Covid-19 were admitted to U.S. hospitals, and immunocompromised patients remained at significantly heightened risk for severe disease.
“This is an important development for the 6.6% of Americans who are immunocompromised — offering the hope of a safer future to those among us who are still most at risk from Covid,” said Matthew Cortland, a senior fellow at Data for Progress and an immunocompromised individual themself, in a text message.
Still, it’s not clear how many patients will avail themselves of the new treatment. Invivyd, the drug’s developer, estimated there are 9 million immunocompromised people in the U.S., but its initial focus will be on the 485,000 with the most acute need: Stem cell transplant recipients, organ transplant recipients, and blood cancer patients.
Evusheld itself had gone vastly underused when it was available, prompting the federal government to launch efforts to educate the public about its existence. And the need is probably less acute now for some: Although immunocompromised patients have a reduced response to vaccination, many may still gain some protection from multiple rounds of vaccination and exposure to the virus. Uptake for other measures to mitigate Covid risk, such as boosters and Paxlovid upon infection, has also declined precipitously, despite public health efforts.
“We will explore having it available at our institution, so that our very compromised patients and the services and specialities that take care of those patients know that it’s an option,” said Priya Nori, an infectious disease specialist at Albert Einstein College of Medicine. “But we’re not expecting gangbusters in terms of interest.”
For Krista Coombs, though, the drug could provide some protection and peace of mind. She said she developed long Covid in early 2020, although it was before diagnostic tests, and has been hit hard with two subsequent reinfections. And last year, she was diagnosed with common variable immune deficiency. (Covid has been linked to persistent immune dysfunction, if not specifically CVID.)
Coombs said the drug wouldn’t radically alter her life, as she still has to work from home and rest often because of persistent fatigue. But she was recently invited to speak about her long Covid advocacy work at Children’s Hospital Los Angeles, and the drug would her make her feel more safe traveling from her home in Bennington, Vt.
“That would help me feel a lot better about flying and being there,” she said. “I’m just thinking ahead, if I want to start doing a bit of things like this, how can I travel and not [fall] sick?”
Combs said, however, that she was concerned about how accessible the drug would be.
Invivyd has not yet disclosed a price, although CEO Dave Hering indicated on a Friday call with investors that it would likely cost more than antibody drugs did during peak Covid, when companies charged around $2,000 per dose. He said Invivyd would charge more because it’s being sold commercially, as opposed to by government purchase, and because, to overcome variants, the company was using a massive dose — several times as much antibody as the Evusheld dose — raising the cost of production.
Hering also indicated the company believed the drug was simply worth more than $2,000.
“We’ve really looked at this from a health economic perspective and what the product could provide,” he said.
The drug can be re-dosed as soon as every three months to increase patients’ antibody levels.
Invivyd was originally founded in 2020 by antibody expert Tillman Gerngross, under the name Adagio, and raised $309 million in an IPO a year later. But the company’s original antibody — which had been designed to be all but variant-proof — was soon rendered ineffective by the advent of Omicron, eventually leading to Gerngross’ resignation and a series of high-level changes at the company.
Pemgarda is a re-engineered version of the original antibody, designed to cover Omicron variants. That gave Invivyd a faster path to getting a new preventative on the market than competitors who started from scratch.
The headline has been updated to note Pemgarda has been given emergency use authorization, not full approval.