How nanotechnology could improve cancer and fertility treatment
May 9, 2024
An advanced robotics lab at Canada’s top university is helping the medical world tackle some of its most perplexing problems – starting at the smallest of scales
This article was originally published on theguardian.com as part of the University of Toronto and Guardian Labs What’s Possible? Ask Toronto campaign.
Advances in treatment and earlier detection have significantly improved cancer survival rates in recent decades. But some cancers remain devastatingly lethal. For patients with glioblastoma (GBM), the most common and aggressive form of brain cancer, the average life expectancy is just 12 to 18 months after diagnosis. Only a quarter will survive more than a year, and just 5% more than five years.
At the University of Toronto, Prof Yu Sun and his team at the Robotics Institute are harnessing the potential of nanorobotics – the field of technology developing microscopically small robots – to build what could be a game changing new treatment option: “nano-scalpels” that seek out cancer cells and destroy them by spinning when activated by a magnetic field.
While chemotherapy is an effective treatment for cancer in the beginning, patients eventually develop resistance to it, and in glioblastoma that happens quickly, says Sun, the founding director of the Robotics Institute. “We hope to give a resort to cancer patients having treatment resistance: can we give them some hope to treat their disease?” he says.
For Sun, the research has a personal resonance: he lost his mother to cancer, and saw first-hand the impact of treatment resistance. “I realised more acutely that patients really need technologies that can help them as the last resort,” he says.
Working with Dr Xi Huang’s lab from Toronto’s Hospital for Sick Children (SickKids), the University of Toronto team developed their “mechanical nanosurgery” by filling magnetic carbon nanotubes – tubular molecules made of carbon – with iron oxide particles and coating them with an antibody that recognises a protein overexpressed by GBM tumour cells. Thanks to the antibodies, when the tubes are injected into a tumour, they seek out cancer cells. Then a precisely applied external rotating magnetic field makes the tubes spin.
“The tubes generate mechanical torque that exerts on cellular structures to mechanically disrupt them and cause cell death,” says Dr Xian Wang, who completed his PhD under Sun, and whose later postdoctoral work was co-supervised by Huang and Sun at the Hospital for Sick Children. Wang’s work developing magnetic nano-tweezers was a building block for the nano-scalpels.
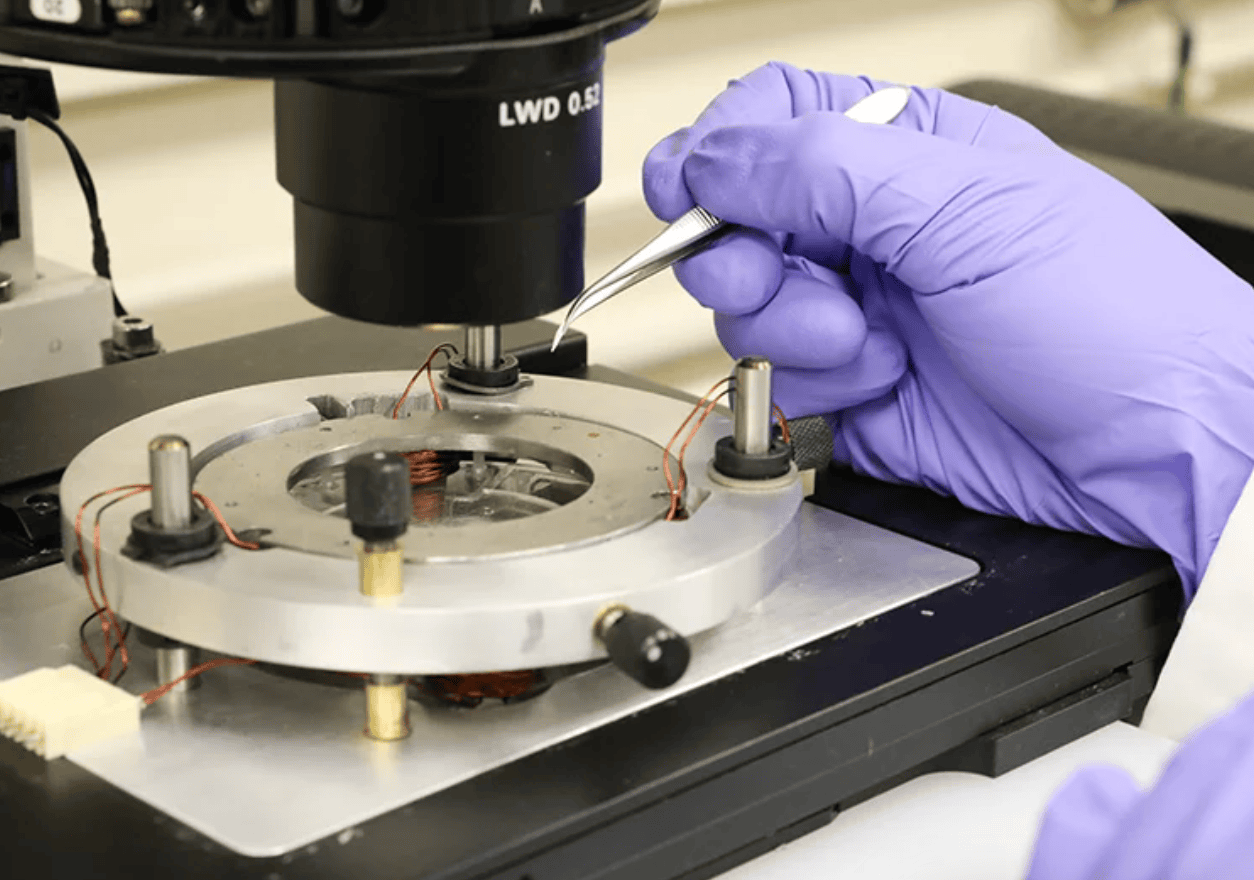
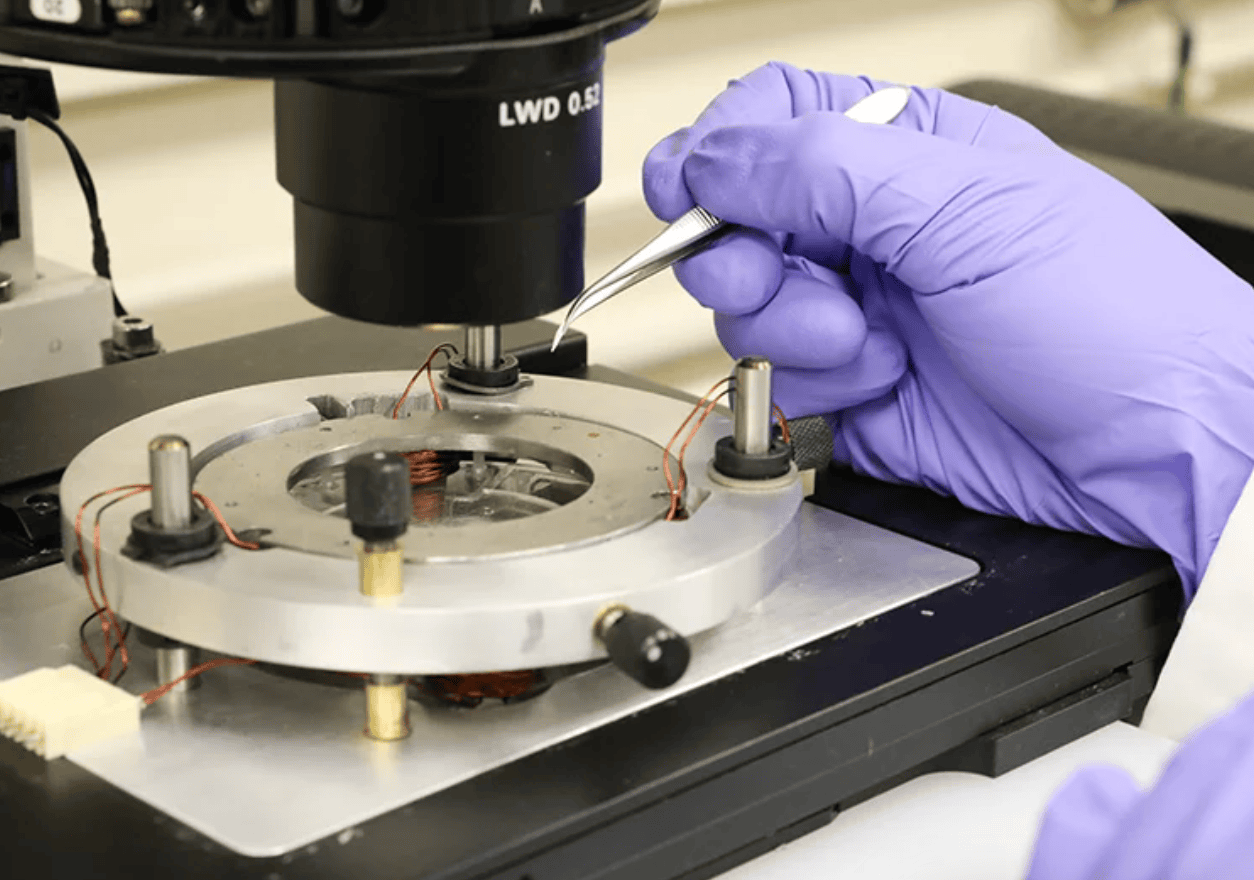
Dr Xian Wang using magnetic coils to control the position of a microscopic carbon nanotube filled with iron oxide. The nanotubes are small enough to enter human cells and can be positioned with unprecedented accuracy. Photo by Tyler Irving.
In a study on mice bearing chemotherapy-resistant GBM, the mechanical nanosurgery reduced tumour size and extended the animals ’survival. The fact that it kills cells physically is crucial, says Wang, now an assistant professor at Queen’s University in Kingston, Ontario, given that treatment resistance occurs because cancer cells mutate to adapt to treatment.
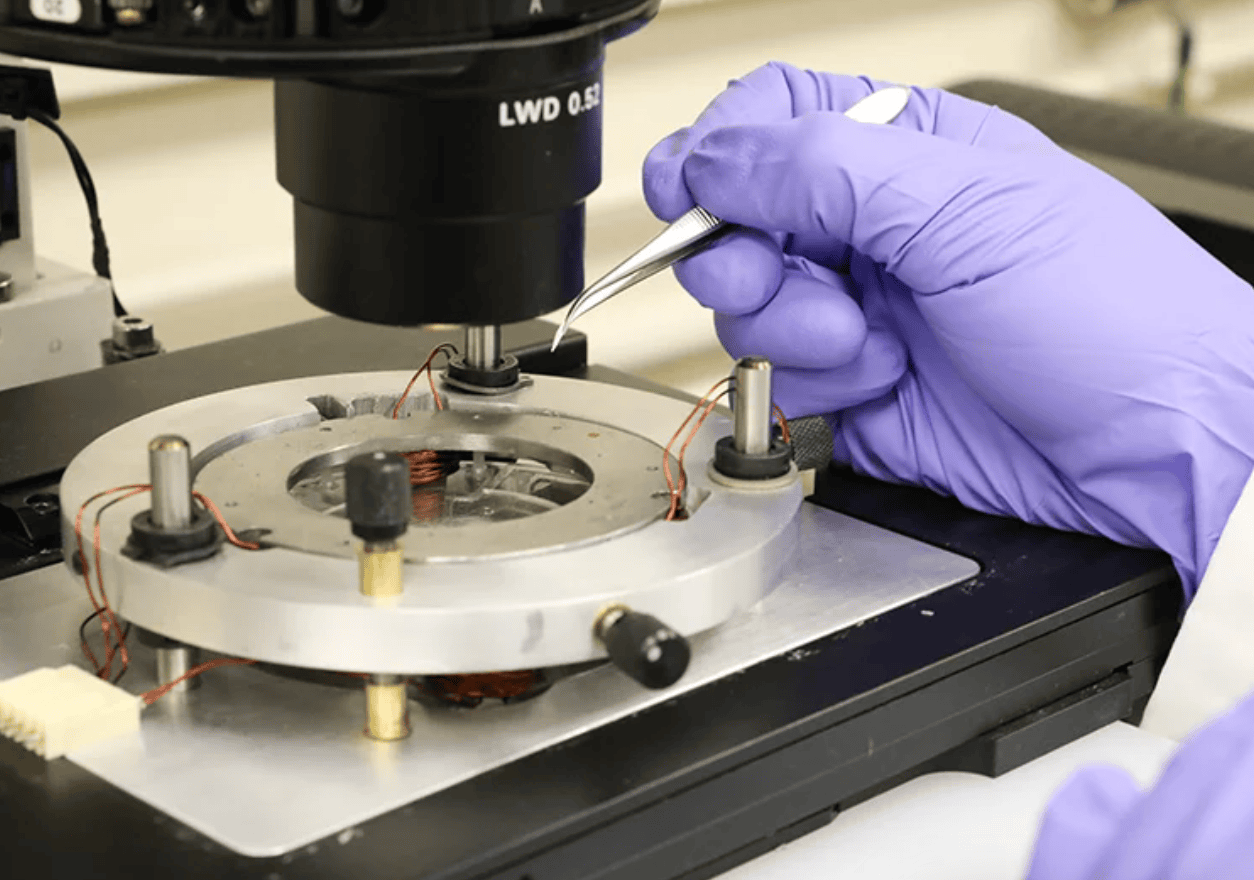
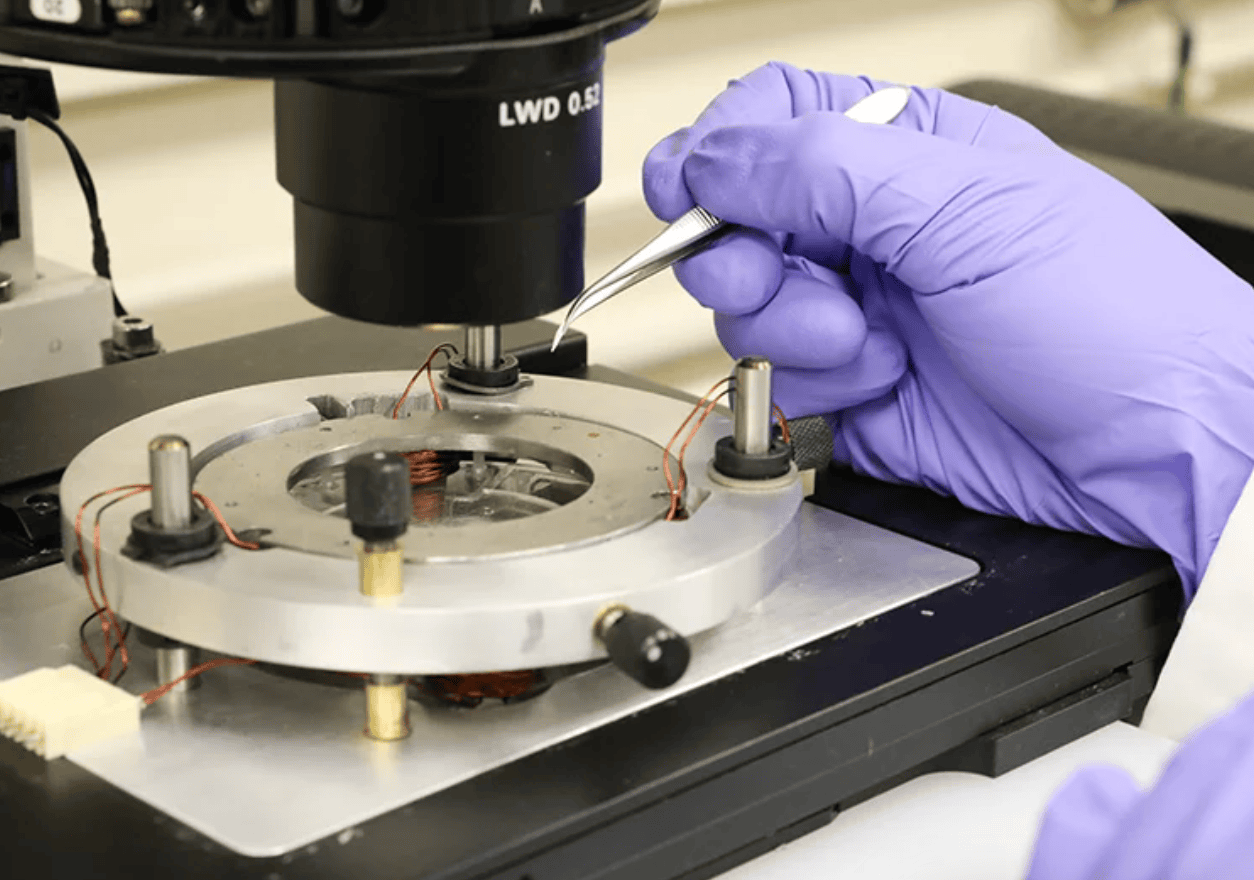
Dr Xian Wang using magnetic coils to control the position of a microscopic carbon nanotube filled with iron oxide. The nanotubes are small enough to enter human cells and can be positioned with unprecedented accuracy. Photo by Tyler Irving.
“The nano-scalpel technology is physical – it doesn’t give the cells the opportunity to mutate, which is why we see it as very important,” says Huang, who played a crucial role in the development of mechanical nanosurgery.
In a more than 20-year career in micro and nanorobotics, Sun has earned a reputation for pioneering work with societal impact. As a graduate student, he wanted his robotic systems working on single cells to have a sense of touch. Unable to find anything that would do the job, he created his own solution: a microforce sensor that went on to be commercially produced and was, among other uses, used by Nasa to optimise the responses of the James Webb space telescope’s microshutters.
He also developed the world’s first closed-loop controlled nanorobotic system, in collaboration with Hitachi High-Tech Canada, which acts as the “hands” alongside an electron microscope as the “eyes” to manipulate and characterise nano-scaled materials and biological samples.
Within healthcare, Sun’s groundbreaking work also focuses on the very beginning of life. At the University of Toronto in 2012, he and his team developed a system that resulted in another world first, this time in automated human fertilisation.


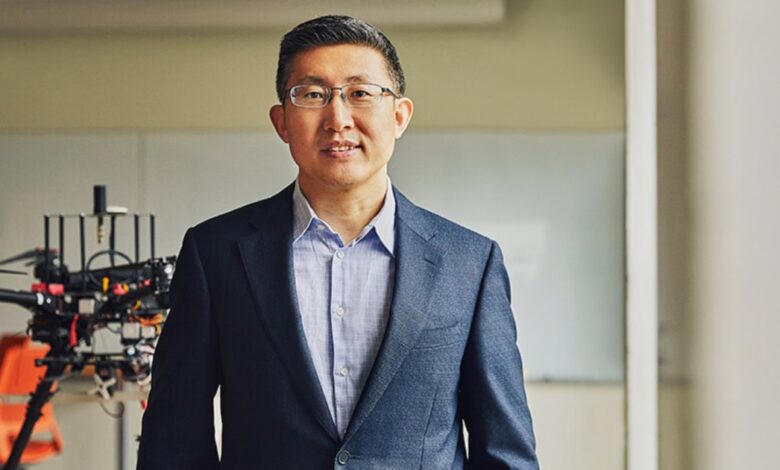
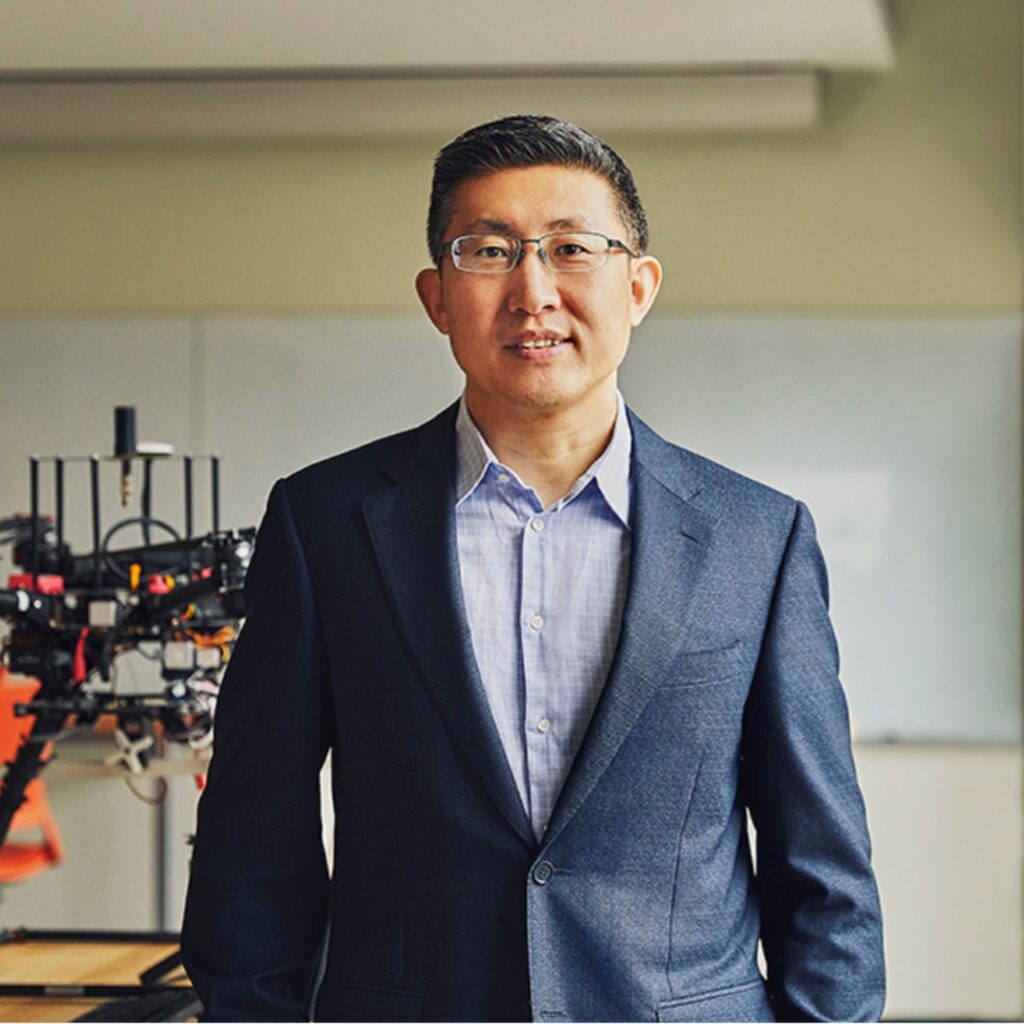
Prof Sun hopes to see the innovations developed at the University of Toronto having real-world effects. Photo by Wei Fang/Getty Images.
Their robotic intracytoplasmic sperm injection (ICSI) system uses painstakingly developed AI algorithms and robotic micromanipulation techniques to non-invasively select sperm with the least DNA damage, then insert them into human egg cells, minimising damage compared with manual methods by using a mechanical vibration device which, says Sun, works “like a woodpecker using mechanical pulses to gently open the egg cell’s membrane”. The aim is to help ensure IVF- born children are healthy.


Prof Sun hopes to see the innovations developed at the University of Toronto having real-world effects. Photo by Wei Fang/Getty Images.
An enhanced version of the system is currently undergoing patient trials. Meanwhile, Sun hopes his team’s mechanical nanosurgery will be ready for clinical trials within five years.
“The pressure of working in this field is not about publishing a paper, but because there are diseases to treat,” he says.
In his working lifetime, he hopes to see his innovations being used with transformative effect in the real world. “I’d love to see the treatment technologies we are working on being used in hospitals to benefit many, many patients,” he says. “Because the purpose of doing the research is to make the world better.”
Meet the extraordinary community that’s pushing the boundaries of what’s possible at utoronto.ca/news
By Rachel Williams



