The potential use of artificial intelligence for venous thromboembolism prophylaxis and management: clinician and healthcare informatician perspectives
Healthcare informatician—respondent characteristics
Of 101 respondents to the healthcare informatician survey, a majority were greater than 40 years old (54.5%), male (62.0%), and white (70.1%) (Table 1). Respondents could identify as more than one role; most were clinicians (44.6%), followed by data scientists (36.6%). Most respondents reported that they had been practicing in informatics for more than 10 years (54.5%).
Most felt they were very well informed (41.6%) or sufficiently informed (48.5%) about AI/ML, with a majority reporting that they had taken coursework on the topic (61.4%) or were doing research on the topic (68.3%). A large portion also reported that they had worked on deploying AI/ML (42.6%).
Clinician survey—respondent characteristics
Of 607 US-based respondents to the clinician survey, a majority were 40 years old or younger (69.9%), female (55.7%), and white (68.2%) (Table 2). Physicians made up 70.7% of respondents, of which 45.4% were trainees. Hospital medicine was the most common specialty (52.1%) followed by hematology (20.8%). A majority of respondents (65.8%) reported making a decision about whether a patient needs VTE prophylaxis every day. Only 20.5% of respondents reported that they had used AI/ML to inform their clinical practice; a majority had not (57.9%) or were unsure (21.6%).
Healthcare informatician—experiences with AI/ML
Most informaticians (62.6%) reported that their organization is using or developing AI/ML for healthcare. Of these 62 respondents, a majority described the status of AI/ML at their organization as implemented with at least one model in use (82.3%), and that their organizations primarily develop the models themselves (81.4%). Less than half (45.8%) reported using third-party vendors or partnering with local universities (28.8%).
Respondents who reported developing AI/ML systems used Python (76.6%), R (45.3%), and toolkits (42.2%). Of the respondents who described what toolkit they prefer, the most commonly cited ones were Scikit-learn and TensorFlow.
Healthcare informatician—attitudes towards AI/ML
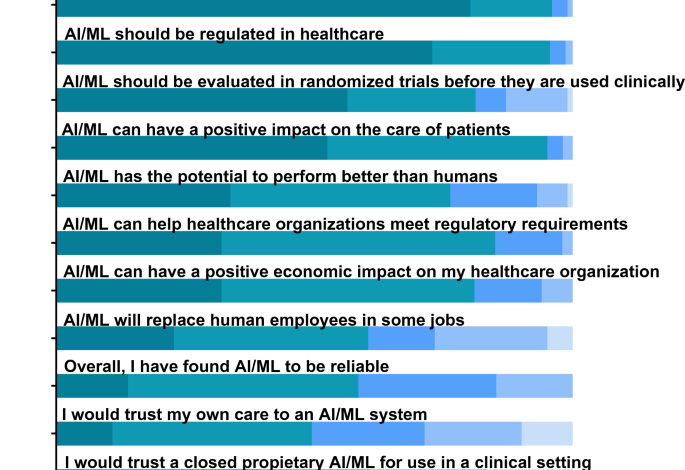
A majority of informaticians agreed that AI/ML can have a positive impact on the care of patients (95.0%), can help healthcare organizations meet regulatory requirements (95.0%), and can have a positive economic impact on their healthcare organization (81.0%) (Fig. 1, Supplementary Table 1). Informaticians mostly agreed that AI/ML has the potential to perform better than humans (76.3%) and will replace human employees in some jobs (60.4%). Respondents found AI/ML to be overall reliable (58.5%) and would trust their own care to an AI/ML system (49.5%). However, less than half would trust a closed proprietary system (39.7%). Most informaticians agreed that AI/ML should be independently vetted and standardized prior to use in a clinical setting (96.0%), regulated (95.6%), and evaluated in randomized controlled trials (81.2%).
The three most common reasons respondents identified as barriers to the successful development of AI/ML in healthcare were data quality (67.3%), lack of standardization (39.8%), and difficulty of acceptance by healthcare providers (35.7%).
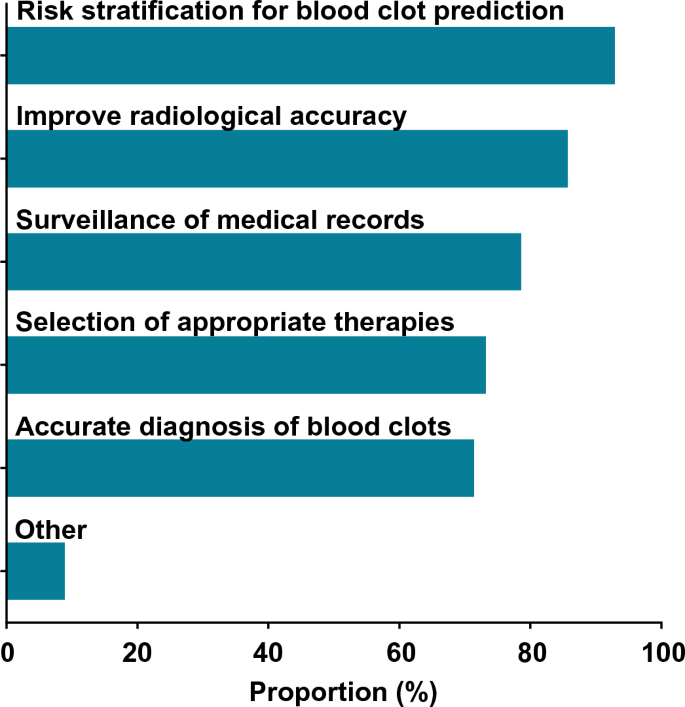
Healthcare informatician—attitudes towards AI/ML for the management of blood clots
A majority of informaticians agreed that AI/ML can be used for clinical management of blood clots (56.0% 95% CI 46–66%). Of these 56 respondents, most agreed that AI/ML can be used for risk stratification (94.6%), radiologic accuracy (87.5%), surveillance (80.4%), diagnosis (73.2%), and treatment (73.2%) (Fig. 2). Four respondents proposed potential additional uses for AI/ML: monitoring the process of clot dissolution, warfarin dosing, shared decision-making, and treatment during acute versus chronic recovery phases. All respondents were asked about perceived barriers, and the most commonly cited barriers were a lack of transparency with AI/ML systems (48.5%), concern that clinicians would not use an AI/ML system (34.7%), and concerns around liability (24.8%) (Supplementary Table 2). Informaticians who identified as clinicians were more likely to think that AI can help with VTE compared to those who did not identify as clinicians, though the difference was not statistically significant (66.7% vs. 47.3%, respectively; p = 0.052). Respondents at organizations that have implemented AI were not significantly more likely to think that AI can help with VTE compared to those at organizations that had not implemented AI (59.0% vs. 48.7%; p = 0.32).
All respondents were asked the free-text question, “What else should be considered when using AI/ML to assist in the clinical management of blood clots?” There were 37 responses, six of which were removed from analysis because they did not answer the questions. Of the remaining 31 responses, nearly all were related to validation of the system and discussed factors related to testing, bias, and transparency. Several responses discussed deployment, and a few responses touched on the importance of clinician oversight (themes in Table 3; coding tree in Supplementary Table 3).